The topic of Wound Care Certification has come up a lot this week as we prepare for the upcoming Wound Care Certification Basic Training.
Rx Pad
2026 Training Course Enrollment is open!
- Hyperbaric Medicine Basic Training
- Wound Care Certification Basic Training
- Hyperbaric Safety Training
- Program Director Training
There are many the benefits of training your team at your facility. Talk to us about creating hybrid learning opportunities combining the ease of livestream and the practical, hands-on learning component of in-person.
Earn 12+ Hyperbaric CME, CEU Hours
Are you looking for hyperbaric-specific CME, CEUs in order to complete your recertification or to fulfill your CME, CEU requirements for hyperbarics?
Physician CME (as per the UHMS Guidelines for Hyperbaric Facility Operations):
"For an initial appointment or reappointment, physicians must complete at least twelve (12) hours of hyperbaric medicine-specific AMA PRA Category 1 CME."
CHT Recertification (as per the NBDHMT):
"Proof of a minimum of 24 (minimum of 12 Category “A”) CEU hours during the prior
two (2) years."
CHS Recertification Requirements (as per the ABWH):
"A minimum of 20 CME credits are required to re-certify. 5 CME credits must be directly related to the practice of hyperbaric medicine."
Attention Physicians: MD and DO, and those who assist them.
Are you clear on the recommended CME's for hyperbaric physicians? Do you know where to go to find critical information regarding the UHMS recommended guidelines for hyperbaric clinic operations? While this is not a "one size fits all" question, we do have some answers for you.
In this article we are uncovering one of the component that make a successful hyperbaric and wound care center by answering the question of, "WHO Needs To Be Involved?"
HYPERBARIC MEDICINE & WOUND CARE TRAININGS
The 2025 January through March training courses are filling up quickly for wound care certification basic training, basic training in hyperbaric medicine, hyperbaric safety director training, and clinic business trainings.
Join us for in-person training for:
Have you ever attended one of our Introduction to Hyperbaric Medicine courses? Last week we had the pleasure of learning from Dr. Michael White, MD, UHM, MMM, CWS who taught Day 2 of the 4-day program.
There are 3 chances left in 2024 to earn your CEU's with us, or complete your trainings in hyperbaric medicine, clinic business, and/or hyperbaric safety . . .
Have you ever attended one of our Introduction to Hyperbaric Medicine courses? Last week we had the pleasure of learning from Dr. Larry Chase, MD, UHM, CWSP who kicked off Day 1 of the 4-day program.
A hyperbaric and hyperoxic environment creates numerous considerations for the use of drug therapies within it. First, the physical stress of hyperbaria impacts drug storage and has implications on which containers are most appropriate for use. Second, physiologic changes to the body from hyperbaria and hyperoxia may lead to pharmacokinetic changes in drug disposition. Lastly, hyperbaric oxygen acting as a drug can interact and enhance or ameliorate the physiologic effect of a drug.
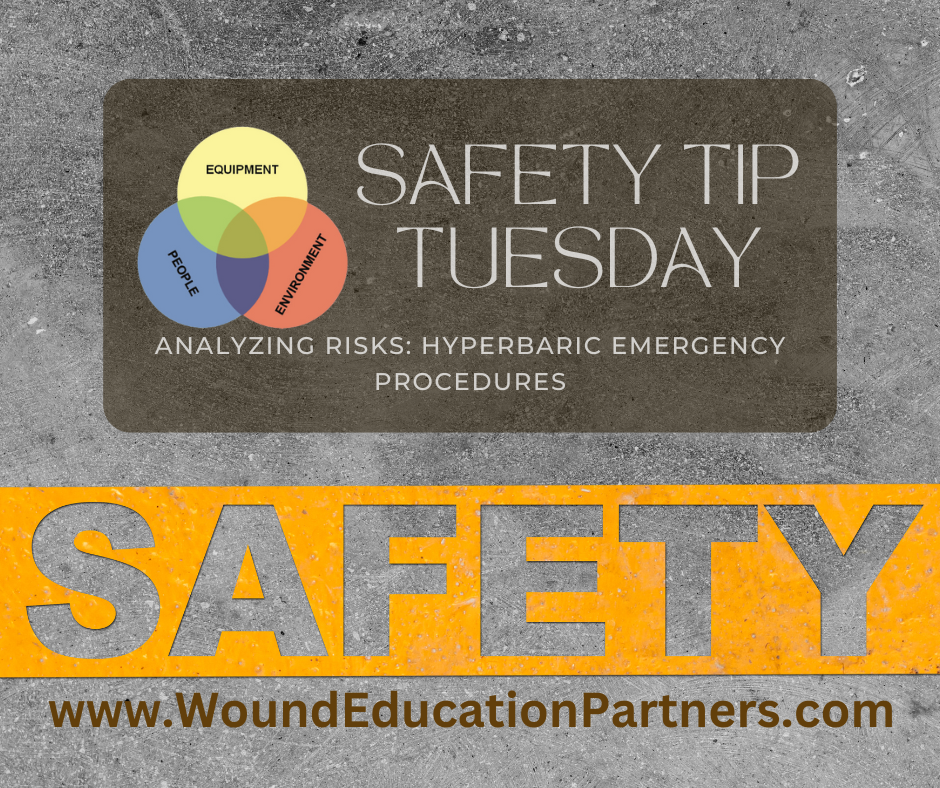
Analysis of hazards and risk assessment allows us to understand the true nature of the potential incident we are attempting to manage. This is an important first step in designing a contingency plan. There are several other important considerations that affect the design of the plan. Realizing the potential damage or injury helps us to identify appropriate staff responses. These responses should minimize the impact of the incident. It is important to consider what personnel are available to help (e.g., additional staff members, code team, and emergency responders) and how these individuals are capable of participating in the plan. Designing contingency plans with available personnel in mind drives minimum facility staffing decisions. It is also important to consider what equipment is available (e.g., personal protection, patient transportation, fire-fighting, and crash cart). All the considerations discussed above are likely to vary among different hyperbaric facilities.
Carbon monoxide exposed patients commonly present with nonspecific symptoms that mimic influenza-like illnesses (Table 1). Symptoms typically include headache, dizziness, nausea, vomiting, weakness, and fatigue . The most common symptom reported is headache . Because these symptoms are so nonspecific, the treating physician must retain a high level of suspicion for carbon monoxide poisoning as delays in recognition and treatment are common .
Carbon monoxide is a colorless, tasteless, and odorless gas. It is one of the leading causes of injury and death worldwide. Based on death certificate data, mortality from unintentional, non-fire-related carbon monoxide exposures results in an average of 439 deaths each year in the United States. However, with improved data collection through the Center for Disease Control, estimates may be closer to 2,000 deaths per year. In 2014, the National Poison Data System listed gases/fumes/vapors as the leading cause of death in children five years old or less. Furthermore, carbon monoxide poisoning results in more than 200,000 emergency department visits per year and more than 20,000 hospital admissions.
Carbon monoxide (CO) originates from incomplete combustion of carbon-containing materials. Common external exposure sources include house fires, automobile exhaust, ice resurfacing machines, furnaces, burning of charcoal, wood, and natural gas for heating or cooking, propane-powered equipment, and methylene chloride paint stripper.
Another major source of CO is cigarette smoking. Average carboxyhemoglobin levels (COHb) of 3 .0%–7 .7% are found in heavy cigarette smokers, compared to 1 .3%–2 .0% in nonsmokers.
Carbon monoxide poisoning can occur occupationally (i.e. firefighters, ice resurfacing machine or forklift operators), unintentionally, and as a means of suicide. The incidence of carbon monoxide poisoning increases during power outages caused by natural disasters. Interestingly, since the introduction of the Clean Air Act in 1970, the mortality rate from motor vehicle–related CO poisoning has declined. Carbon monoxide is also produced endogenously through the degradation of hemoglobin by heme oxidase, resulting in detectable carboxyhemoglobin levels in nonexposed individuals.
In industry, the major factor for carbon monoxide exposure is inadequate ventilation where propane-powered vehicles are used. Exposures from forklifts and ice resurfacing machines have been reported. Other work environments that produce large amounts of CO, and therefore heighten the risk of poisoning, are the steel industry, due to coke ovens, and the paint industry, in which inhaled methylene chloride (dichloromethane) is metabolized to CO by the liver. Firefighters and other first responders are also at increased risk for CO poisoning from smoke inhalation and from entering environments with elevated CO levels unknowingly.
Men have higher rates of death from carbon monoxide poisoning, presumably due to higher risk behaviors and environments. The elderly (age ≥ 65) are also at increased risk for death from CO poisoning as they are more likely to dismiss symptoms as being caused by underlying medical conditions more prevalent in this population.
Women and children, however, are more likely to be exposed to carbon monoxide, and most exposures occur in the winter months (November to February).
Source Reference: Excerpted from Hyperbaric Medicine Practice 4th Edition with permission from the publisher. Reference Chapter 13, Carbon Monoxide by Jillian Theobald
Learn More
Are you seeking basic training in hyperbaric medicine? Our UHMS and NBDHMT approved 40-hour Introduction to Hyperbaric Medicine training course will teach you and your team the key fundamental elements and concepts in practicing hyperbaric medicine safely and effectively. Find your course today! https://www.woundeducationpartners.com/live-courses/hbo-courses.html
In this third and final installment of How Accidents Happen we continue looking at personnel & management as contributing factors in hyperbaric facility accidents.
In this installment of How Accidents Happen we continue looking at personnel & management as contributing factors in hyperbaric facility accidents.
When one commences a task to reconstruct how an accident happened, personnel and management factors are often “at the head of the class.” Some of the more commonly occurring factors are discussed in this section. It should be noted, however, that this list is not all-inclusive. The factors that can contribute to accidents are many and varied. As technology and operations become ever more complex, our ability to create new ways to “do ourselves in” are amazing.
For some accidents there is a clear “smoking gun.” However, most accidents are caused by a combination of factors, each of which contributes in some manner. Often these factors accumulate over some period of time preceding the accident. This chapter addresses the factors that foster conditions under which accidents are more likely to happen and discusses some of the steps to be taken to avoid them. Also included is a case history illustrating several of the factors.
Type of Acrylic Windows used in Hyperbaric Multiplace and Monoplace Chambers
In today’s clinical and diving hyperbaric chambers, acrylic windows with PVHO-1 defined standard geometries and design criteria are used.1 Acrylic window shapes vary with chamber type and the window requirement of the specific chamber type.
Determining the best interventions, including dressing selection, for patients and their wounds requires looking at the situation holistically. Creating the treatment plan for a chronic wound is dependent upon many diverse patient, wound, economic, and social considerations. The dressing selection goes beyond simply choosing a product to cover the wound. Detailed assessments of the patient and wound should drive the components of goal-directed wound care. The health-care provider must determine the etiology of the wound, patient comorbidities that may impair the wound healing processes (e.g. diabetes and blood glucose levels), nutrition/hydration status, systemic and local tissue oxygenation, and patient/family concerns such as pain and odor issues. Each of these factors contributes to creating an individualized plan of care for choosing the most appropriate products and interventions.
Analysis of hyperbaric facility risks is a difficult process. It begins with identifying the hazards in a hyperbaric facility. These hazards could be from a variety of sources: equipment related (e.g. loss of power, loss of gas supply, control system malfunction); operational (e.g. untrained or unprepared staff); medical (e.g. pressure injuries, medical complica- tions); and environmental (e.g. contaminants, external disaster). The actual risks associated with a hazard depend on the probability, frequency, and severity of the potential losses.
Hyperbaric emergency procedures usually address a variety of problems ranging from mechanical malfunction to medical complications—important events that do not seem to share a common trait but cover a wide range of situations. Such a variable group of events must be discussed in a broad context. This chapter will discuss emergency pro- cedures within the framework of the entire hyperbaric safety program. In this broader context, events that may or may not be emergencies belong together. That is why this dis- cussion will replace the term “emergency procedure” with the term “contingency plan.”
A consensus document by Keast et al. reviewed clinically useful wound measurement approaches. This evidence-based document provided an overview of principles and practice regarding chronic wound assessment in a simple mnemonic format. The text articulated effective management of a nonhealing wound based upon:
Various theories have been proposed to explain why some wounds become chronic and non-healing. Although the complete answer is not yet available, a great deal has been learned in recent years that sheds light on this phenomenon.
In the past several years, there has been rapid growth in the number of clinical hyperbaric facilities, due in part to the availability of the monoplace, or single-person, hyperbaric chamber and the proliferation of outpatient wound care centers. Monoplace chambers are relatively inexpensive, require fewer personnel, and require less space to operate and maintain than multiplace (walk-in) chambers. Another advantage of the monoplace over the multiplace chamber is that attendants need not enter the hyperbaric chamber with the patient. However, some hyperbaric physicians express concerns about treating unstable or critically ill patients in the monoplace chamber, because of the lack of “hands-on” care during hyperbaric exposure, the lack of suitable equipment for optimal patient care, and the limitations of treatment pressures to 3 atmospheres absolute pressure (ATA). We have found that with a well-trained staff and the availability of appropriate equipment, critically ill patients can be treated safely in the monoplace chamber. We, and others, have presented monoplace chamber use in critically ill patients. Anyone who anticipates treating critically ill patients in a monoplace chamber should be familiar with this work.
Adequate wound perfusion and its delivery of oxygen to the healing tissues is fundamental to wound healing as just explained. Revascularization invariably is the first intervention considered to achieve this goal. Hyperbaric oxygen all too often is not considered in the management. In addition, other interventions can improve perfusion-oxygenation. These include edema reduction, improvement in cardiac function through medical management, and enhanced blood rheology using pharmacological methods. In contrast to the other four treatment strategies where typically a single technique is utilized, the methods to improve the perfusion-oxygenation strategy are complimentary, and typically two or more techniques are employed simultaneously.
The second source of information regarding perfusion-oxygen needs for wound healing arises from indirect information . It is obvious that markedly increased blood flow and oxygen availability are required to heal a wound and control infection.(19) Perfusion and oxygen requirements are minimal for noncritical tissues that do not have wounds or infections because they are in a steady-state, resting status. An example of this would be the feet of the patient with advanced peripheral artery disease. If a relatively minor wound occurs in one foot, healing may not occur, and a lower limb amputation becomes necessary. In contrast, in the opposite limb that does not have a wound, but perfusion is equally poor, the foot is not immediately at risk for an amputation.
In general, fire prevention is described in terms of the Fire Triangle model. For a fire to occur, a fuel, an oxidizer, and an ignition source must be present. Fire prevention in a hyperbaric chamber must account for an increase in the oxygen component of the atmosphere in terms of both oxygen fraction and partial pressure. The resultant increase in oxygen renders what might be inactive fuels and ignition sources in a “normal” air environment active, which increases the risk of a fire.
Wound oxygenation is an essential strategy for the management of wounds regardless of their severity. Fortunately, in most wound healing situations, autoregulatory mechanisms ensure that oxygen is adequate to meet metabolic requirements. When not adequate, wound healing may be impeded or even totally interrupted, infection may not be controlled, and tissues may die, leading to limb amputations . Wound oxygenation is a function of perfusion. This part of the three-part series discusses oxygen requirements for wound healing and control of infection and methods (and their rationale) for augmenting wound perfusion-oxygenation and introduces the subject of hyperbaric oxygen (HBO2) as a tactic for mitigating hypoxia in wounds in particular and in other conditions where HBO2 is useful in general.
Safety in a hyperbaric chamber begins with design and specifications that are incorporated in construction codes such as the ASME Boiler and Pressure Vessel Code. ASME and related codes establish minimum standards for materials utilized in the construction of a chamber and how those materials are fabricated.2 Subcodes address specific requirements for pressure vessels intended for human occupancy and the viewports utilized in the chamber.3 ASME codes focus on maintenance of the structural integrity of the chamber during routine operations as well as providing safety components such as pressure relief valves to reduce the potential for catastrophic failure of the chamber in the event of overpressure resulting from fire or other mishap. A chamber will undergo inspection, testing, and be stamped to indicate that it has been manufactured in compliance with the applicable pressure vessel code. In many locales, only stamped pressure vessels are allowed to be utilized.
There are differing opinions regarding when to use advanced wound modalities. Many believe that advanced wound modalities should only be used when a wound fails to heal with standard wound management over some period of time, while some believe that advanced therapies should be used immediately on wounds that are identified to be potentially difficult to heal.(2-6) Most insurance carriers have specific guidelines that govern when they will allow use of advanced wound modalities.
For some accidents there is a clear “smoking gun.” However, most accidents are caused by a combination of factors, each of which contributes in some manner. Often these factors accumulate over some period of time preceding the accident. This chapter addresses the factors that foster conditions under which accidents are more likely to happen and discusses some of the steps to be taken to avoid them. Also included is a case history illustrating several of the factors.
Dressing product selection is based on comprehensive assessments of the wound and the patient’s overall physiology. Determining whether a person’s body can support complete wound healing requires clinical skills and significant knowledge of the many barriers to healing, including which impediments can be influenced by the wound care team and which cannot. When making decisions for treatment, one should consider whether the wound has healing potential, is more likely maintenance wound, or has evolved to a non healable ulcer unable to garner the endogenous constituents needed for wound closure and healing.(12,16) For instance, a patient with end-stage cancer who has a Stage 4 infected pressure injury located on the sacrum may benefit from interventions aimed at pain and odor control, addressing the infection, support for activities of daily living, and other health-related quality-of-life issues addressed through a palliative care approach rather than aggressive debridement and advanced dressings looking at the end goal of wound closure.(16) In such a case, maintenance wound care would be more appropriate.
Copyright
© Wound Care Education Partners
Determing the best interventions, including dressing selection, for patients and their wounds requires looking at the situation holistically. Creating the treatment plan for a chronic wound is dependent upon many diverse patient, wound, economic, and social considerations. The dressing selection goes beyond simply choosing a product to cover the wound. Details assessments of the patient and wound should drive the components of goal-directed wound care. The health-care provider must determine the etiology of the wound, patient comorbidities that may impair the wound healing process (e.g. diabetes and blood glucose levels), nutrition/hydration status, systemic and local tissue oxygenation, and patient/familiy concerns such as pain and odor issues. Each of these factors contribute to creating an individualized plan for care for choosing the most appropriate products and interventions.
Copyright
© Wound Care Education Partners
In this 3 - Part series, we're looking at the most commonly used classification scales currently in use to classify diabetic foot ulcers, including:
There are many scales that attempt to classify diabetic foot ulcers, but few have been validated and none have demonstarated prognistic reliabilty or accuracy with regard to healing a DFU. Some scales focus on anatomy (depth of ulcer), some include vasular assessment, and others include the presence or absence of infection.
Diabetes mellitus is an epidemic of global proportion with a steadily rising prealence of disease. There were an estimated 28.9 million (21 million diagnosed, 8.1 million undiagnosed) adults with diabetes mellitus in the United States in 2012. The prevalence of diabetes mellitus among adults has quadrupled from 1980 to 2014. This rate continues to rise, with 1.7 million new cases reported in 2012. Globally, it is estimated that there are 422 million adults with diabetes mellitus.
This is the third and final installment in the series about how to prepare your patient for wound care treatment.
This is the second in the series about how to prepare your patient for wound care treatment. In Part 1 we covered Transfers, Patient Comfort, Pain Scales; if you missed Part 1, you can read it here
In this series we're going to breakdown the main techniques to comfort patients when preparing for wound care treatment.
Have you ever heard the term "casting a wide net" when it comes to marketing? It's referring to the need to get your message in front of a huge number of prospective referral sources if you want to get a lot of patient referrals coming in.
Starting in 2018 Centers for Medicare and Medicaid {CMS} Services in conjunction with the American Medical Association {AMA} recognized the need to reduce documentation requirements for providers (physicians and non-physician practitioners). In 2019, the History component consist of three requirements of Chief Compliant (CC) {reason for the visit}, History of Present Illness {HPI} and Review of Systems (ROS) noting information needs to relevant to the Chief Compliant. They approved of allowing the patient, caregiver, or ancillary staff to document the patient’s History in conjunction that the provider would review the information for relevancy while also documenting the provider reviewed stated patient information at the visit.
Copyright
© Wound Care Education Partners
Question: I am interested in adding hyperbaric oxygen therapy to my clinic. What are your recommendations for staff education and management of hyperbaric medicine in my clinic?
Answer: The first step we recommend is that you attend a 40-hour UHMS and NBDHMT approved basic training in hyperbaric medicine course, Introduction to Hyperbaric Medicine. Wound Care Education Partners offers the course many times per year across the U.S., and we could also do onsite training at your facility.
Upcoming course dates and locations can be found at the following link https://www.woundeducationpartners.com/live-courses/upcoming-courses.html
As for management, we recommend that you attend our Business of Wound Care and Hyperbaric Medicine course. This 16-hour CME/CEU course guides you through the administration of operating and managing a profitable wound care/hyperbaric clinic. This course is offered a few times per year at various locations across the U.S.
Find upcoming courses at the following link: https://www.woundeducationpartners.com/live-courses/the-business-of-wound-care-and-hyperbaric-medicine.html
For more information on any of our courses please contact us at
Various theories have been proposed to explain why some wounds become chronic and nonhealing. Although the complete answer is not yet available, a great deal has been learned in recent years that sheds light on this phenomenon.
Case study - Edema
History: This patient presents to the wound care clinic with a history of alcohol abuse, tobacco use, and congestive heart failure. Patient states that her legs are prone to swelling.
South Florida in winter . . . doesn't that sound great?!
Let’s face it . . . with clinic budgets being tight, it can be really hard to request funds to attend a conference.
This Friday, January 27 at 12:00 Noon EST we are hosting a live free webinar information session to discuss affordable solutions for hyperbaric staff training.
Copyright
© Wound Care Education Partners